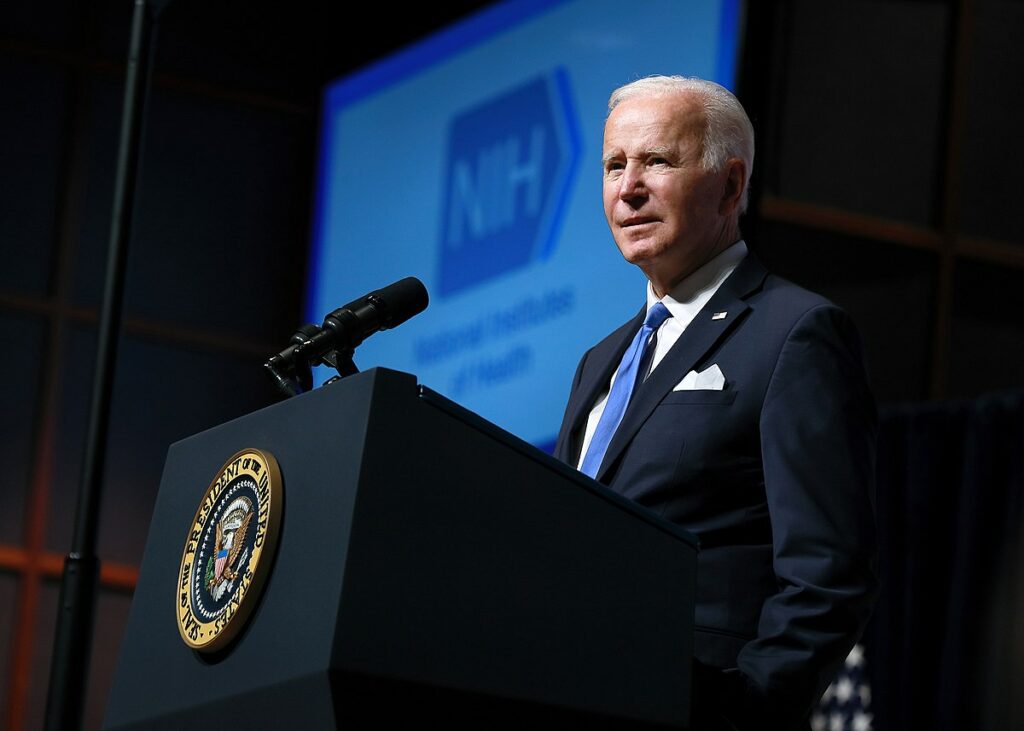
US President Joe Biden has stepped into a long-running debate about whether the National Institutes of Health (NIH) has legal authority to override an exclusive patent license granted to drug developers if they charge too much for treatments that relied on agency-funded research. In draft policy guidance, the Biden administration says federal agencies would be able to use so-called “march-in” rights when a company is not charging a “reasonable” price for a product. https://www.science.org/content/article/biden-wants-nih-have-march-power-override-patent-rights-high-priced-drugs?
The “proposed framework” was released last Thursday as part of other White House actions aimed at the high drug prices that have become a sore point for politicians and the public. It would clarify that a tool for removing patent protection to ensure a government-funded invention is commercialised can be used for an overly pricey drug so that other companies can sell it more cheaply. Although consumer advocates and lawmakers are hailing the proposal, some of them worry it sets an impossibly high bar for determining when a price is reasonable.
Drug companies and academic institutions are expected to oppose it, arguing any such actions by NIH will dissuade industry from developing and commercialising treatments based on taxpayer-funded research. The Pharmaceutical Research and Manufacturers of America trade group, noting that companies fund most costs of drug development, called the proposal “a road map for seizing patents” and “another loss for American patients and inventors.”
March-in rights originated in the 1980 Bayh-Dole Act, which allows academic institutions to patent inventions made using NIH or other federal grant funding and grant exclusive licenses for companies to develop them. The law states that if an invention is not being commercialised or otherwise made accessible to the public, the government can march in and make the patent-holding institution license its invention to additional companies.
Consumer and patient groups have argued that NIH should exert its march-in rights for drugs it deems inaccessible to some U.S. patients because of high prices. Petitions have demanded the agency act on the HIV drug ritonavir and, more recently, the prostate cancer drug enzalutamide (sold as Xtandi), for example. The latter costs about $160,000 a year in the United States, five to six times the cost in Canada and Japan. But NIH has never exercised its march-in rights, despite at least seven petitions to do so over more than 2 decades.
On a press video call yesterday, NIH’s director, Monica Bertagnolli, briefly addressed the topic, saying: “I will use every tool I possibly can with the goal of obtaining the access [to drugs] that our patients need. … And if I am to ever apply [march-in rights], it will be according to principles that allow it to really achieve that specific aim.”
In early 2021, as part of a potential revision of the Bayh-Dole Act, then-President Donald Trump’s administration proposed preventing agencies from exercising march-in rights solely on the basis of price. In March, however, Biden declined to do that and instead formed an interagency working group force to review the march-in issue with the Department of Commerce’s National Institute of Standards and Technology (NIST).
///
https://www.science.org/content/article/tumor-killing-viruses-score-rare-success-late-stage-trial?
Once touted as the next big thing in cancer therapy, tumour-attacking viruses have been a let-down, failing in multiple clinical trials as far back as 1949. But preliminary results from a small phase 3 study presented at a conference last month suggest these unconventional cancer treatments, known as oncolytic viruses, might work after all. The data showed that an oncolytic virus developed by Irvine, California–based CG Oncology eliminated tumours in 64% of 66 patients with bladder cancer that didn’t respond to mainline treatment.
The follow-up period was only 6 months, and much more research is necessary. But even a positive phase 3 result is enough to “shake the world of oncolytic viruses,” says surgical oncologist Omeed Moaven of the Louisiana State University Medical Centre. And if the promise shown in these early data holds up, the oncolytic virus could become only the second in the United States to receive regulatory approval, a milestone that would bode well for the dozens of other trials now underway. Success would also vindicate a strategy of designing the viruses to draw an immune attack on the tumour rather than only hitting malignant cells directly.
The viruses—usually benign varieties such as the herpes simplex viruses and adenoviruses that are often modified to make them safer and more potent—can reproduce in tumour cells but not in healthy cells. Cancer cells are congenial for the viruses because they frequently shut down the first line of defence—known as the interferon response—against viral infections.
Doses of the viruses worked beautifully in animal studies, sometimes achieving 100% cure rates. But after more than 70 years of clinical trials around the world, only T-VEC, a modified herpes simplex virus type 1 (HSV1) that targets advanced melanoma, has performed well enough to receive the Food and Drug Administration’s go-ahead. (And other melanoma therapies work better for most patients.) Three other oncolytic viruses were okayed outside the U.S., most recently a treatment for glioma brain tumours was approved in Japan in 2021.
Virologist Mary Hitt of the University of Alberta cites one reason for the clinical trial failures. At first, “everyone was afraid they wouldn’t be safe.” As a result, she says, many trials used weakened viruses that were too feeble to do much good. Another problem was that researchers didn’t understand how oncolytic viruses worked.
Scientists once thought that “these viruses were magic bullets” that killed tumour cells directly, says immunologist Greg Delgoffe of the University of Pittsburgh. But through animal studies and analyses of tumour samples from patients treated in clinical trials, researchers realised that the viruses themselves take out relatively few tumour cells. Instead, oncolytic viruses rile the immune system, triggering inflammation and attracting anticancer warriors such as T cells, and they help break down the defences that shield tumours. That picture helps explain the early failures. Participants typically had already undergone several rounds of therapies that could inhibit their immune systems.
A slew of companies is now trying to apply these lessons and turn oncolytic viruses into therapies, and more than 90 clinical trials are testing them or are about to start. CG Oncology’s virus—a harmless adenovirus—is one contender. The company outfitted it with a gene that spurs infected cancer cells to produce an immune-stimulating molecule, promoting attacks by T cells.
The phase 3 trial tested the virus in patients with a form of bladder cancer that hadn’t penetrated the muscular wall of the organ. If tumours like these grow unchecked, patients often need to have their bladders removed, but the virus may delay or prevent that outcome. Doctors assessed the participants every 3 months after the treatment began. In 76% of the patients, tumours were undetectable at one or more of these check-ups. And in 74% of that group, the tumours did not return for at least 6 months.
“It’s an interim analysis, but what we’ve seen is a good start,” says urologic oncologist Mark Tyson of the Mayo Clinic, who has several patients enrolled in the trial and unveiled the findings at the Society of Urologic Oncology conference. Researchers will track the patients for a total of 3 years to determine whether the benefits persist, says Tyson, who has no connection to CG Oncology.
Other candidate oncolytic viruses may soon get their chance. For example, neurosurgeon E. Antonio Chiocca of Brigham and Women’s Hospital and his colleagues are testing an engineered HSV1 against glioblastoma, a type of glioma that usually kills patients in less than 2 years. In previous efforts to pit this virus against glioblastoma, scientists removed a gene essential for viral reproduction, hoping to prevent brain inflammation, a possible side effect of the treatment. But the modification also left the virus “attenuated,” Chiocca says.
Instead, he and his team used a version of the virus with the gene restored, but it was engineered to switch on only in glioblastoma cells. This version was safe, the researchers found in a phase 1 trial with 41 patients whose tumours had returned after surgery or other treatments. The virus also allowed T cells to invade the tumours. The more T cells entered, the longer the patients survived, the scientists reported in October in Nature.
////
Japanese regulators have approved a COVID-19 vaccine constructed using a form of RNA that can make copies of itself inside cells. It’s the first ‘self-amplifying’ RNA (saRNA) vaccine platform to be granted full regulatory approval anywhere in the world. Because it could be used at a lower dose, it might have fewer side effects than other messenger RNA (mRNA) treatments have. When used as a booster in clinical testing, the newly authorised vaccine, ARCT-154 — developed by US biotechnology firm Arcturus Therapeutics and Australia-based CSL — triggered higher levels of virus-fighting antibodies that circulated the body for longer than did a standard mRNA COVID-19 vaccine.
////
Your major organs can age at different rates — and organs that look old before their time are linked to disease risk. Researchers identified proteins that originated mainly from a single organ and trained a machine-learning algorithm to match the levels of these proteins with age. When a person’s levels differed substantially from other people of the same age, it spelled trouble: for example, an ‘old’ heart was linked to a 250% increased risk of heart failure.
Nature | 4 min read
Reference: Nature paper
////
Lalita Panicker is Consulting Editor, Views and Editor, Insight, Hindustan Times, New Delhi

