A long-simmering scientific battle assumed a new life this week, as experts clashed in a San Francisco courtroom over whether the U.S. Environmental Protection Agency (EPA) should ban fluoridation of drinking water to protect foetuses and children from the risk of neurodevelopmental problems. https://www.science.org/content/article/does-fluoride-drinking-water-lower-iq-question-looms-large-court-battle?
The case, being heard in a federal district court, “is precedent setting,” says Lynn Bergeson, a managing partner of Bergeson & Campbell who focuses on chemical toxicity. Rarely have judges had to “manage the enormity of this record of scientific evidence. … That’s why there’s a lot of attention focused on this right now.”
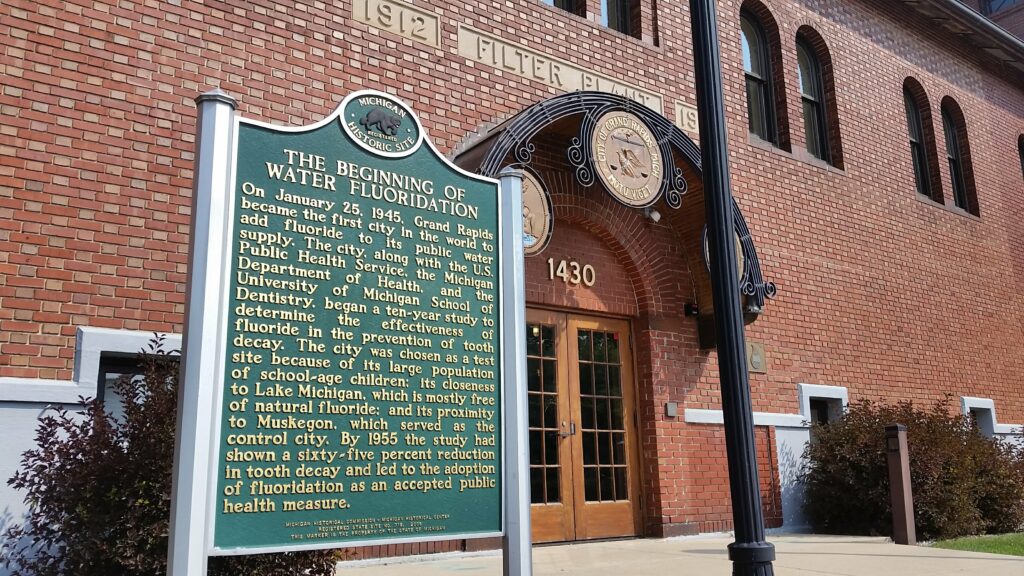
Adding fluoride, a common mineral, to drinking water lessens tooth decay in children and adults by 25%. The US Centers for Disease Control and Prevention (CDC) calls fluoridation, one of 10 “great public health achievements” of the 20th century. It began in 1946 in the United States and is decided by local water districts, But from the start, some activist groups worried about potential harm. And over the past few decades, studies of laboratory animals and of communities where drinking water naturally contains fluoride have hinted that high levels might affect brain development.
The current case has put the spotlight on an unpublished assessment by the federal government’s National Toxicology Program (NTP). It reported “moderate confidence” that drinking water containing fluoride at levels at least twice as high as those recommended by the federal government is associated with lower IQ in children. The Fluoride Action Network (FAN) and other groups argue that such data indicate EPA should be regulating fluoride under the Toxic Substances Control Act (TSCA).
This week’s testimony marked the resumption, after a yearslong pause, of litigation that began in 2017. Over 9 days, Judge Edward Chen of the U.S. District Court for the Northern District of California is scheduled to hear the views of seven experts on a range of technical topics, including whether there is a safe threshold for fluoride exposure.
Chen has suggested that EPA must regulate fluoride if FAN proves that fluoride poses an “unreasonable risk” to pregnant women and children. Under TSCA, EPA cannot consider a chemical’s benefits, such as oral health.
Lynn Goldman, an epidemiologist at George Washington University and former EPA official, doubts that Chen will order EPA to ban fluoride in drinking water. “I can’t imagine a court coming back and saying, ‘You did a risk assessment wrong, and here’s how you should have done it,’” she says. But the court might order EPA to consider fluoride as a toxic substance under TSCA and make it a high priority for a new evaluation to establish safe exposure limits.
////
An experimental pain reliever that could offer a non-addictive alternative to opioids showed efficacy in two large, pivotal trials. The compound, called VX-548, aims to sidestep opioids’ lure and other side effects by blocking a sodium channel called Nav1.8 on pain-sensing neurons. www.science.org/content/article/nonopioid-drug-candidate-relieves-acute-pain-large-trials?
The phase 3 trials were designed to follow up on promising results from two smaller studies, in which VX-548 provided better relief than a placebo for acute pain after surgeries to remove bunions or excess abdominal fat. The new studies enrolled 1073 bunionectomy and 1118 abdominoplasty patients, randomized to get either VX-548, a placebo, or a combination of acetaminophen and the opioid hydrocodone.
Those getting VX-548 reported more pain relief in the first 48 hours after surgery than those in the placebo arm, which means the trial hit its primary endpoint, its maker, Vertex Pharmaceuticals, reported in a press release. But the VX-548 recipients reported less relief than those who got acetaminophen and hydrocodone. (Vertex and its academic partners had defined superiority to that drug combo, widely known as Vicodin, as a secondary trial endpoint.) The company hopes the new results will support regulatory approval of VX-548 to treat moderate to severe acute pain and plans to file its application to the U.S. Food and Drug Administration by mid-year. Earlier stage trials are evaluating VX-548 against chronic pain, a more complex set of conditions for which fewer effective treatments are available.
////
The World Health Organization (WHO) last week gave emergency use approval to a low-cost COVID-19 vaccine, years after observers questioned whether regulators in India rushed to authorize its use there without sufficient evidence. www.science.org/content/article/news-glance-mars-helicopter-s-final-flight-grants-u-k-diversity-and-nonopioid-pain-drug?
Corbevax, a vaccine based on part of the coronavirus’ spike protein, was developed at Texas Children’s Hospital and Baylor College of Medicine and is notable because its developers didn’t seek patent protection on it. In 2020 they freely licensed it to Biological E Limited, a global vaccine supplier based in India. In December 2021, the Drugs Controller General of India gave emergency use authorization for adults and later greenlighted it for adolescents and as a booster. Biological E was able to sell the two-dose vaccine to the government at the extraordinarily low price of 145 rupees ($1.90) per dose, and people in India have received more than 100 million doses. It is the 14th COVID-19 vaccine to receive an emergency use listing from WHO, whose endorsements often influence whether a low-income country considers a vaccine.
////
Cancer surgeon Dr Andre Ilbawi says he’s haunted by the memory of a patient in Kenya whose suffering made him “want to scream so loud that you would lose your voice.”
The woman was just 37 years old. But her breast cancer was so advanced that by the time Ilbawi encountered her in a hospital outpatient clinic in 2019, her death was imminent. www.npr.org/sections/goatsandsoda/2024/02/01/1228089751/the-breast-cancer-burden-in-lower-income-countries-is-even-worse-than-we-thought?
Ilbawi, who is the World Health Organization’s lead expert on cancer, was in Kenya on a personal trip to volunteer in his capacity as a surgeon. He says what made witnessing the woman’s situation all the more terrible was a galling thought: If she had lived in a wealthy country such as the United States, it was highly likely her tumour would have been caught far earlier – giving doctors enough time to save her.
“To look at her and imagine that in a different place, she could have been cured of her cancer and lived a full and abundant life,” he says. “The injustice of it is indescribable.”
This week Ilbawi nonetheless attempted to convey at least some of the scale of the global inequities around breast cancer care, with the release of the latest worldwide statistics compiled by the World Health Organization.
The data are assembled every two years by officials of WHO’s cancer agency and are used to estimate the incidence and death rates of 36 types of cancers in 185 countries. Ilbawi and other WHO officials say among the most “striking” findings in this year’s report are the figures pointing up the outsized burden of breast cancer on low-income countries.
Cancer is actually far more common in wealthy countries than in lower income ones. Ilbawi says that’s largely because women in lower income nations have less exposure to risk factors such as obesity and alcohol consumption. They also tend to have more children – which reduces the chance of breast cancer. The upshot: While in the highest income nations one woman out of every 12 will be diagnosed with breast cancer in her lifetime, in the lowest income nations the figure drops to one in 27.
Yet a woman who develops breast cancer in a lower income country is so much more likely to die of it than if she were in a wealthier nation. So the disease is a much bigger cause of women’s death in lower income countries. In the wealthiest countries 1 in 71 women will die of breast cancer. In the lowest income countries, 1 in 48 women will die of it.
////
Lalita Panicker is Consulting Editor, Views and Editor, Insight, Hindustan Times, New Delhi

